Understanding Perinatal Anxiety: Symptoms, Causes, and Healing for Birthing People & Families
Becoming a parent is often portrayed as a time of joy and fulfillment, but for many, the perinatal period (pregnancy through the first year postpartum) is marked by overwhelming anxiety. While some stress is normal, clinical perinatal anxiety disorders go beyond typical worries, affecting a parent’s well-being, their family, and even their baby’s development.
In this post, we’ll explore:
The symptoms of perinatal anxiety disorders
Factors that contribute to them
The difference between normal stress and clinical anxiety
The far-reaching impacts on parents, infants, and society
Evidence-based treatments and holistic approaches
Why systemic change is necessary for true prevention
What Does Perinatal Anxiety Feel Like? Personal Stories and Symptoms
Imagine this:
Sarah, a first-time mom, can’t stop imagining worst-case scenarios. What if she drops her baby? What if he stops breathing in his sleep? She checks his chest repeatedly at night, her heart racing. She avoids leaving the house, fearing something terrible will happen. Her partner tells her, “You’re overreacting,” but the dread feels inescapable.
Perinatal anxiety isn’t just “worrying a lot.” It’s persistent, intrusive fear that disrupts daily life. Symptoms may include:
Intrusive thoughts (unwanted, distressing mental images)
Physical symptoms (racing heart, nausea, dizziness)
Hypervigilance (constant scanning for danger)
Avoidance behaviors (skipping outings, excessive Googling)
Sleep disturbances (even when the baby is asleep)
Unlike fleeting concerns, these symptoms don’t ease with reassurance.
What Causes Perinatal Anxiety?
While hormonal shifts play a role, anxiety arises from a combination of factors:
Biological: Family history of anxiety, sensitivity to hormonal changes. (1)
Psychological: Perfectionism, trauma history, low emotional tolerance. (2)
Social: Lack of support, financial stress, relationship strain. (3)
Systemic: Inadequate parental leave, healthcare barriers, societal pressure to “bounce back”. (4)
When Does Normal Stress Become Clinical Anxiety?
All new parents experience stress, but clinical anxiety:
Persists (lasting weeks or months)
Impairs functioning (difficulty caring for self or baby)
Feels uncontrollable (reassurance doesn’t help)
Example:
Healthy stress: “I’m nervous about labor, but I trust my care team.”
Clinical anxiety: “I can’t sleep because I’m convinced I’ll die in childbirth.”
The Ripple Effect: How Perinatal Anxiety Impacts Birthing people, Babies, and Families
On Perents…
Chronic anxiety can lead to exhaustion, isolation, and depression. Many parents suffer silently, fearing judgment. The constant state of hypervigilance leaves little room for rest or self-care, making even small daily tasks feel overwhelming. Over time, untreated anxiety can erode self-esteem and make bonding with their baby more difficult.
On Infant Mental Health…
Infants and their primary caregivers operate as a dyad—a connected unit. Research shows that maternal anxiety can affect:
A baby’s stress response: Babies of anxious mothers may have elevated cortisol levels, making them more reactive to stress. (5)
Attachment security: Insecure attachment can develop if a mother is emotionally unavailable due to anxiety, affecting the child’s future relationships. (6)
Cognitive and emotional development: Studies suggest that prolonged exposure to maternal anxiety may correlate with delays in language and emotional regulation. (7)
As psychologist D.W. Winnicott said, “There is no such thing as a baby… only a baby and someone.” This underscores how deeply interconnected parental and infant well-being truly are.
Economic and Societal Costs…
The U.S. loses $14 billion annually from untreated perinatal mood disorders (8). This includes lost productivity, increased medical costs, and higher rates of disability claims. Workplace policies lacking paid leave further exacerbate parental stress (9). Parents forced to return to work too soon face impossible choices between financial stability and recovery or worsening mental health outcomes.
How U.S. Culture Fuels Perinatal Anxiety
Individualism: Parents are expected to “do it all” without communal support, leading to burnout and shame when they inevitably need help.
Capitalism: The pressure to return to work quickly worsens stress, as many parents can’t afford unpaid leave or fear professional repercussions.
Social Media: Unrealistic portrayals of parenthood create shame, making caregivers feel inadequate when their experience doesn’t match curated online narratives.
Compared to countries with robust parental support (e.g., Scandinavia), the U.S. has higher rates of perinatal anxiety (10).
Experts attribute this to:
Weak social safety nets: Without guaranteed healthcare or parental leave, birthing people bear disproportionate stress.
Medicalized, rather than holistic, perinatal care: Overemphasis on biomedical interventions can neglect emotional and social needs.
Stigma around mental health: Many parents avoid seeking help due to fear of being labeled "unfit."
What Happens If We Ignore Perinatal Anxiety?
Untreated anxiety can lead to:
Chronic mental health struggles: Anxiety left unaddressed often evolves into long-term disorders like generalized anxiety or OCD.
Relationship breakdowns: Partners and family members may struggle to support a parent in distress, leading to conflict and isolation.
Long-term effects on child development: Children of anxious parents are at higher risk for anxiety themselves, perpetuating an intergenerational cycle.
Higher healthcare costs: Emergency room visits, prolonged therapy, and lost work hours create a financial burden on families and systems.
Healing Perinatal Anxiety: Evidence-Based and Holistic Approaches
Gold-Standard Therapies
Cognitive Behavioral Therapy (CBT): Challenges thought distortions by identifying and reframing irrational fears (e.g., "I'm a bad parent" → "I'm doing my best").
Exposure Therapy: Reduces avoidance behaviors by gradually confronting feared situations (e.g., taking the baby outside despite anxiety).
Acceptance and Commitment Therapy (ACT): Builds emotional resilience by teaching mindfulness and value-driven action, even amid discomfort.
Medication and Talk Therapy Combined: Medication can aid in decreasing the severity of the symptoms of anxiety enough to allow a parent to actively participate and do “the work” in talk therapy—regardless of the therapy approach.
Complementary Approaches
Mindfulness & Meditation: Helps ground anxious thoughts in the present moment, reducing rumination.
Support Groups: Isolation worsens anxiety, while shared experiences normalize struggles and foster connection.
Body-Based Therapies (yoga, somatic experiencing): Anxiety lives in the body; these practices release tension and regulate the nervous system.
Addressing the Root: Emotional Avoidance and Thought Patterns
Anxiety thrives when we…
Avoid discomfort. Suppressing emotions amplifies them; therapy teaches tolerance.
Believe we “can’t handle” emotions. Building distress tolerance is key to breaking the anxiety cycle.
Struggle with uncertainty. Learning to accept "not knowing" reduces the need for control.
Engage in catastrophic thinking. CBT helps challenge worst-case scenario thinking.
Therapy helps parents reframe unhelpful thoughts and build skills to navigate anxiety without avoidance.
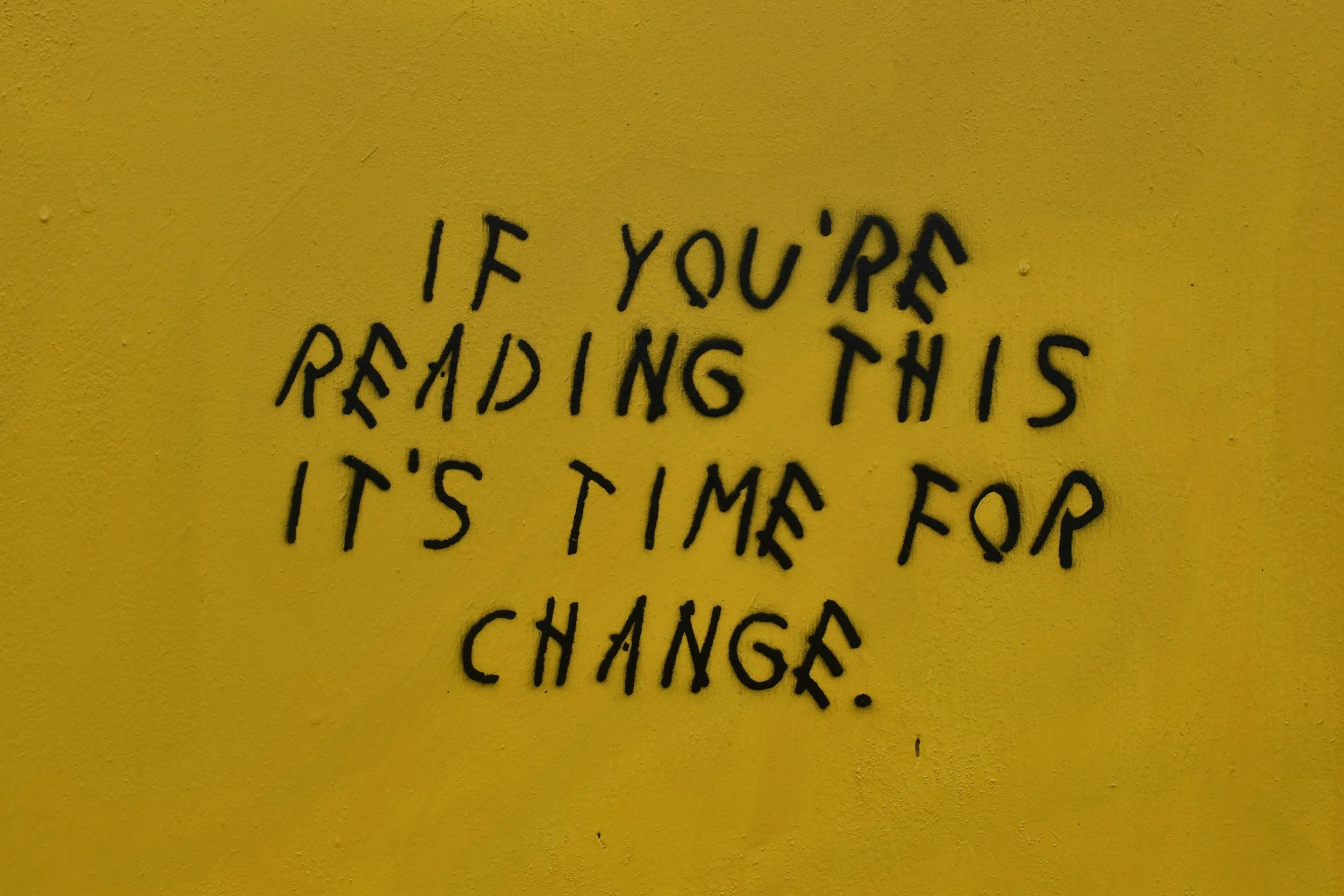
Why Treatment Isn’t Enough: The Need for Systemic Change
Even the best therapies can’t counteract:
No paid parental leave: Financial instability forces parents back to work before they’re physically or emotionally ready.
Lack of affordable childcare: Without reliable care, parents face constant stress about balancing work and caregiving.
Healthcare inequities: Marginalized communities often lack access to quality perinatal mental health care.
Prevention-Focused Solutions
Policy Changes: Mandate paid leave, subsidize childcare, and expand Medicaid for postpartum care.
Community Care: Postpartum doulas, peer support programs, and home-visiting nurses can bridge gaps in care.
Cultural Shifts: Normalize parental struggles by sharing real stories and reducing stigma around help-seeking.
Final Thoughts: A Call for Compassion and Change
Perinatal anxiety isn’t a personal failing—it’s a societal one. While therapy helps individuals, we must also demand systemic support for parents.
If you’re struggling, know this: You are not alone, and help exists. Reach out to a perinatal mental health specialist today.
Additional Resources For Families Struggling:
Postpartum Support International | https://postpartum.net/
Text “Help” to 800-944-4773 (EN)
Text en Español: 971-203-7773
Lifeline Suicide & Crisis Hotline | Call/Text 988
CoAbode - Communal Housing For Single Mothers | https://www.coabode.org/
Sources:
American Psychological Association (APA)
National Institute of Mental Health (NIMH)
World Health Organization (WHO)
Centers for Disease Control and Prevention (CDC)
Journal of Child Psychology and Psychiatry
Attachment & Human Development
Infant Mental Health Journal
Maternal Mental Health Leadership Alliance
U.S. Department of Labor
Cross-Cultural Research in Perinatal Mental Health
This blog is original content written for Beyond The Birth, LLC. If you wish to share or republish, please credit appropriately.
For more resources, visit https://www.beyondthebirth.co/
Beyond The Birth, LLC specializes in perinatal mental health, offering therapy that recognizes the political roots of parental stress. We are in network with several private insurance plans and offer affordable tiered private pay fees for services. Return to our home page on this site to learn more.